With the COVID-19 crisis, there is much talk about the importance of testing to see if you have the coronavirus and if you possibly have immunity to it. But what’s the difference between testing for COVID-19 and testing for its antibodies?
THE QUESTION: Is there any difference between a test for COVID-19 and the test to see if you have antibodies to the coronavirus?
THE ANSWER: Yes. The COVID-19 test looks for active disease. The antibody test is an after-the-fact test that shows your body fought off the disease. Also, they are administered differently.
WHAT WE FOUND: The PCR (polymerase chain reaction) test, the most common for finding out if you have COVID-19 now, starts with a long swab reaching into the back of your nose or throat, where RNA particles of the coronavirus would collect. In the lab, the PCR test is positive if it finds the RNA of the virus. Also called a molecular or nucleic acid-based test, it can find COVID-19 before you feel any symptoms -- and before you form antibodies.
The serologic antibody test uses blood to find out if you’ve had COVID-19, even if you never felt sick. This test looks for markers of an immune response – the antibodies – which for most people show up in blood about a week after they contract the coronavirus.
“They detect the body’s immune response to the infection caused by the virus rather than the virus itself,” the Food and Drug Administration says.
In other words, “if you have a positive antibody test, it means that at some point, the patient has been exposed to the virus,” said Dr. Michael Borowitz, executive deputy director of pathology at Johns Hopkins University and laboratory director of Johns Hopkins Hospital.
For a consumer, Dr. Borowitz said, the antibody tests requiring blood drawn from your arm, not taken from a finger prick, are generally more reliable.
The hope is that people who have the antibodies can resume normal life and return to their jobs – especially those in health care and emergency response and at nursing homes, where staffers with immunity could reduce COVID-19 among frail residents.
But some cautions about immunity: First, because COVID-19 is new, it’s only an assumption that people with antibodies will have immunity.
The test “doesn't tell you just because a patient has an antibody that he’s necessarily immune to the disease. That's what everyone wants to know, but that hasn't been proven,” Dr. Borowitz said.
But if people do have immunity, the next question is for how long?
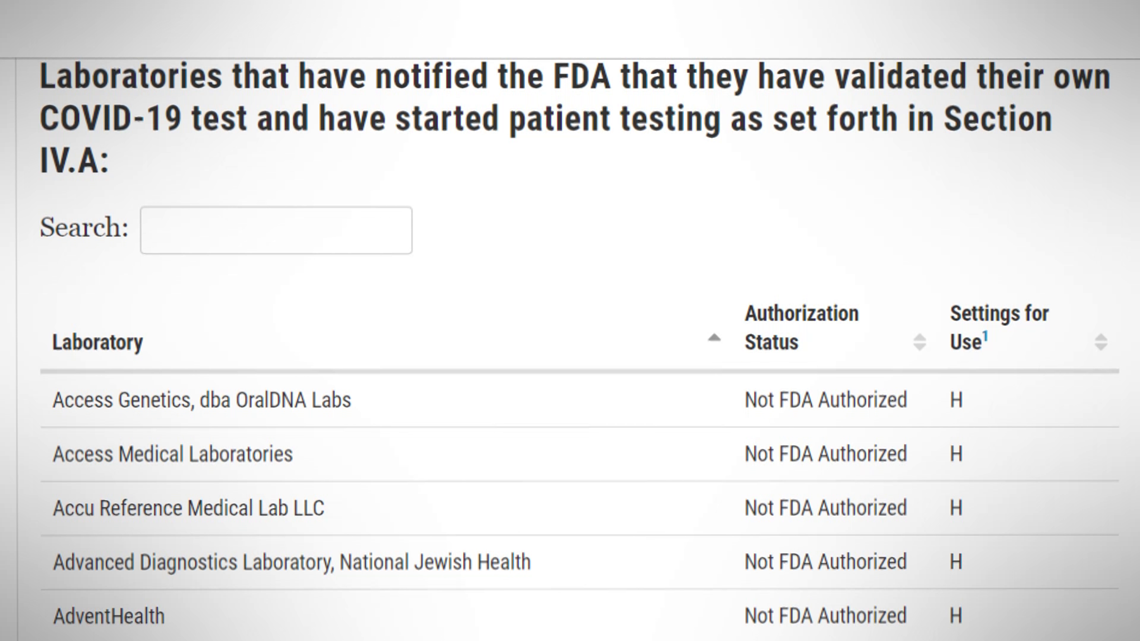
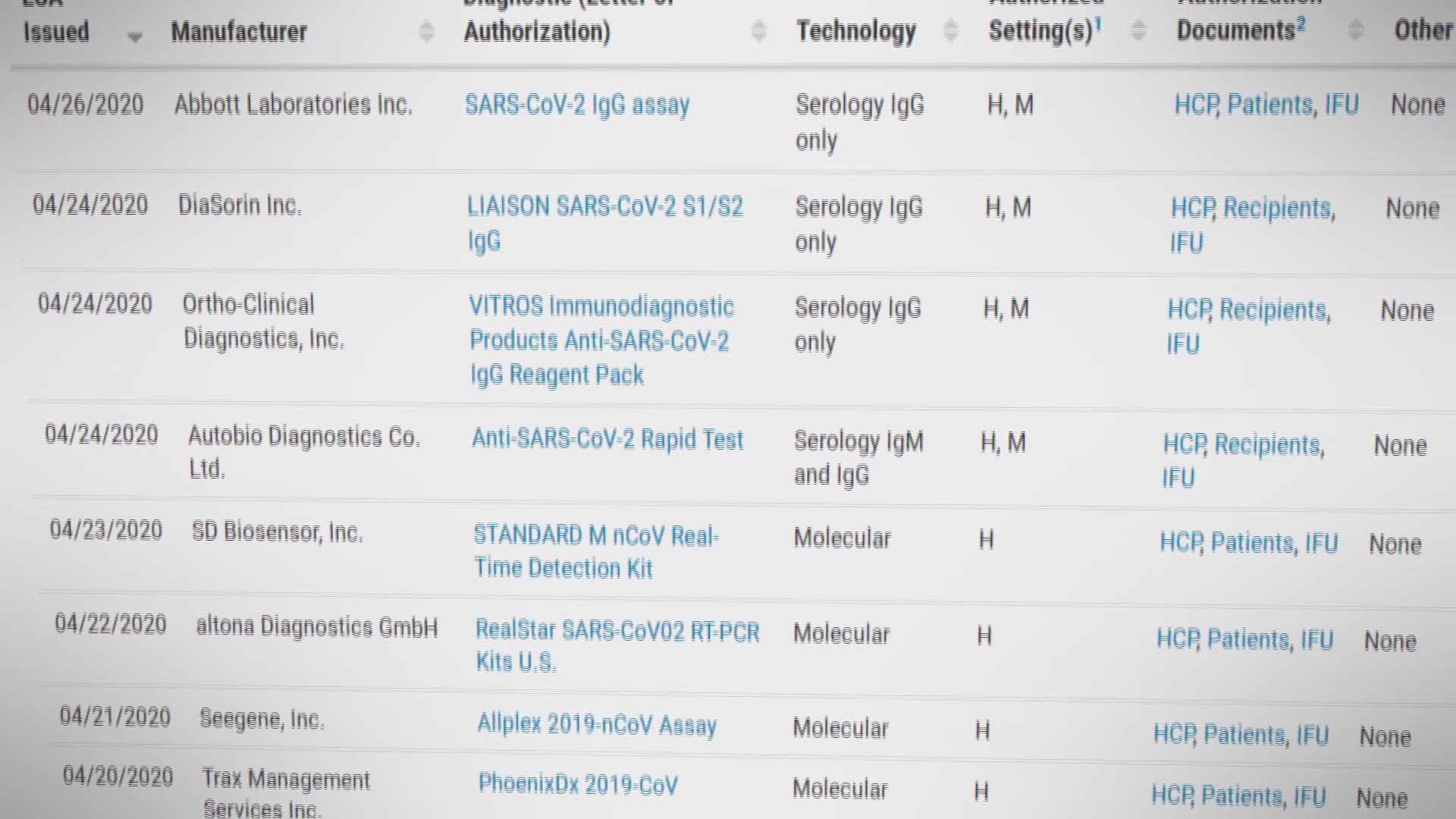
Also, be aware that the FDA has given “emergency use authorization” to only one home test for diagnosing COVID-19 and, as of April 22, only four antibody tests for use by health care providers.
In fact, the FDA warns that “some test developers falsely claim their serological tests are FDA approved or authorized.” A test with the emergency authorization, a sort of preliminary approval, or a National Institutes of Health evaluation “supports greater confidence in test performance,” it says.